Heart failure can be a scary diagnosis. But what if there’s something else going on that’s even harder to spot?
Meet transthyretin cardiac amyloidosis (ATTR-CM)—a serious heart condition that is difficult to diagnose. While it affects both men and women, diagnosis can be more challenging for women.1
This is partially due to gender gaps women face in healthcare generally. Overall, women can face delays in getting proper medical care and receive delayed diagnoses (on average, four years later) compared to men across 770 types of diseases.2
So, what is ATTR-CM and why is it challenging to diagnose? ATTR-CM can lead to a number of symptoms that people think are due to aging but in reality are due to the accumulation of amyloid fibrils in the heart and other organs.3 Here’s how the condition develops: your body makes a protein called transthyretin (or TTR for short) which helps transport vitamin A (retinol), and a hormone called thyroxine throughout the body.4 In some people, due to age (wild-type ATTR-CM) or genetic factors (hereditary ATTR-CM), TTR can become unstable and break apart.5 When it does, it can misfold and accumulate in long strands called amyloid fibrils.5 In ATTR-CM, these fibrils build up in the heart causing the heart muscle to become thick and stiff and lead to heart failure.5,6 The fibrils can also accumulate in other organs too.5 Over time, ATTR-CM continues to progress resulting in deteriorating organ function, reduced quality of life, and can ultimately be fatal.5,7 An early diagnosis is important to slow down further disease progression and potentially improve outcomes.5

Faye’s Story: A Journey Through Misdiagnosis
In 2018, Faye, now a 44-year-old stay-at-home mom to two boys, started experiencing unsettling changes like rapid weight gain, extreme fatigue, and fluid retention in her legs. Despite visiting several specialists over two years, the South Carolina resident still didn’t have a clear diagnosis.
Initially, Faye didn’t make the connection between her symptoms and those experienced by her father, who was diagnosed with ATTR-CM. As his caregiver, she knew firsthand the distressing impact of this heart condition—which can be hereditary in some cases.5
As her condition worsened, a concerned cardiologist ordered several tests, including an electrocardiogram (ECG), which can detect irregularities in heartbeat, and an echocardiogram (echo), which checks the structure and function of the heart.8,9 The tests came back abnormal and showed thickness in her left ventricle, one chamber of the heart. Finally, the doctor ordered a pyrophosphate (PYP) test and a genetic test. The PYP test injects a small amount of Tc-PYP tracer, scans your body, and shows if amyloid is in your heart.10 The genetic test looks for mutations in the TTR gene.5 The PYP scan confirmed her diagnosis of ATTR-CM. Faye felt devastated. A genetic test confirmed she carried the same mutation that had taken her father. Overwhelmed, she initially struggled to share it with her husband Brad, fearing a similar downward spiral.
“It felt like a death sentence,” Faye explains. “In 2010, my father passed away at 57 from hereditary ATTR-CM. All I could see was his journey.”
But Brad refused to give in to despair. He encouraged Faye to focus on the positive. She got diagnosed earlier than her father did. And with Brad’s unwavering support, Faye found the strength to keep fighting.
Faye eventually connected with a doctor who listened and worked with her to develop a comprehensive disease management plan. Slowly, Faye began to regain hope for the future. Now, she’s determined to use her experience to educate others about the critical importance of early ATTR-CM diagnosis.
Recognizing the Red Flags of ATTR-CM
It can take roughly four years from the time of symptom onset to ATTR-CM diagnosis, with people seeing multiple physicians before receiving a diagnosis.11 Catching the disease before it reaches later stages is crucial, allowing patients to get the most out of treatment.5
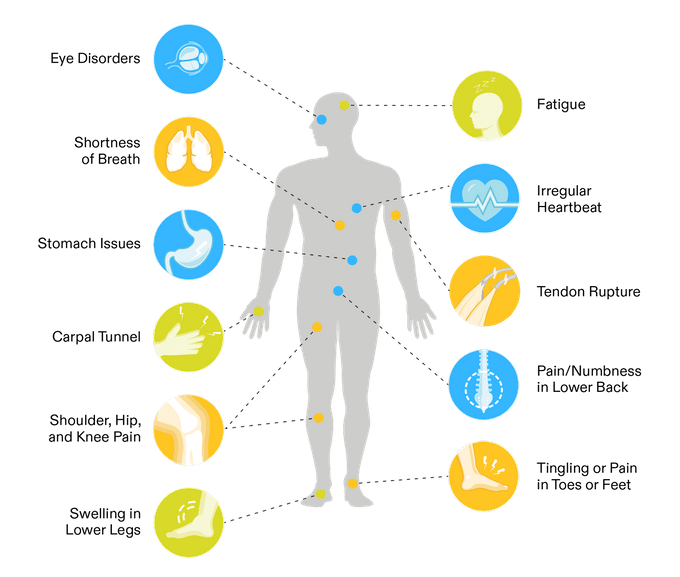
While ATTR-CM is a heart condition, sometimes the signs that show up don’t seem heart-related.5 People with heart failure may notice unresolved issues like carpal tunnel syndrome, lower back pain (spinal stenosis), or tingling or numbness in lower limbs.5 Think of them as non-heart-related red flags. But if you’re experiencing any of these symptoms along with heart problems—such as fatigue, shortness of breath, or irregular heartbeat—it’s important to see a doctor.5 Early diagnosis is important with this progressive and fatal disease.
Women and ATTR-CM: A Gender Gap in Diagnosis
The multifaceted nature of ATTR-CM makes it easy to overlook, especially in women, who are often believed to be at lower risk.12,13 And while ATTR-CM is more common in men, it’s important to pay attention to nuances in women that can hint at the disease, notes Dr. Marianna Fontana, professor of cardiology at the University College London and honorary consultant cardiologist at the National Amyloidosis Centre. Women may exhibit different signs than men, and hormonal factors together with social biases in healthcare settings further compound the problem.14,15,16
Dr. Fontana and her team conducted a large study to compare men and women with ATTR-CM. They found that while men and women show similar heart issues on initial scans, women tend to be diagnosed later when the disease is more advanced.17 Anatomical differences in the female heart can also make ATTR-CM harder to detect.14
“The current methods for diagnosing thickening of the left ventricle, one chamber of the heart where the wall becomes thicker than normal, in men and women are flawed because the same wall thickness cutoffs are used for both genders,” explains Dr. Fontana. “Since women tend to have naturally thinner walls, this can lead to delayed diagnosis or underdiagnosis in women.”
Being diagnosed at a later, more advanced stage of the disease can dramatically impact a person’s prognosis.13 According to one study, women have a decreased length of survival from diagnosis compared to men—27.9 months for women versus 43.5 months for men—suggesting missed and later diagnoses are impacting clinical outcomes for women.18 Early diagnosis is critical so people can make an appropriate disease management plan with their doctor earlier, to potentially slow disease progression and improve outcomes.13

Empowering Yourself: Taking Action
Women may face greater challenges when it comes to getting properly diagnosed for ATTR-CM—a serious heart condition. This can slow the path to establishing a disease management plan.
If you, or someone you love, are living with heart failure and unresolved symptoms, don’t brush them off—and don’t give up! Advocate fiercely for yourself and your loved one. Talk to a doctor about your risk for ATTR-CM, and push for the comprehensive testing needed to catch this disease early. Get a second opinion from a cardiologist who specializes in cardiac amyloidosis if needed.
Not sure where to start? Visit YourHeartsMessage.com and view the Doctor Discussion Guide to help you navigate your next appointment.
“There’s much more hope now than there ever was,” notes Faye. “For me, having a terminal illness is life-changing. And it can take you in two directions. I’m thankful for my husband and my family and my faith that pull me in the right direction. Every day I wake up, it may be a struggle—but there’s still hope in every day.”
References
1Fragner, M., Elsaygh, J., Srivats, S. S., & Pink, K. (2024). Gender Differences in the Evaluation and Management of New Acute CHF Due to ATTRwt Cardiac Amyloidosis. Cureus, 16(4), e59058. https://doi.org/10.7759/cureus.59058
2Westergaard, D., Moseley, P., Sørup, F.K.H. et al. (2019). Population-wide analysis of differences in disease progression patterns in men and women. Nat Commun 10, 666. https://doi.org/10.1038/s41467-019-08475-9
3Irabor, B., McMillan, J. M., & Fine, N. M. (2022). Assessment and Management of Older Patients With Transthyretin Amyloidosis Cardiomyopathy: Geriatric Cardiology, Frailty Assessment and Beyond. Frontiers in cardiovascular medicine, 9, 863179. https://doi.org/10.3389/fcvm.2022.863179
4Wu, D., & Chen, W. (2024). Molecular mechanisms and emerging therapies in wild-type transthyretin amyloid cardiomyopathy. Heart Failure Reviews, 29, 511–521.
5Jain, A., & Zahra, F. (2023). Transthyretin amyloid cardiomyopathy (ATTR-CM). In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK574531/
6Ruberg, F. L., Grogan, M., Hanna, M., Kelly, J. W., & Maurer, M. S. (2019). Transthyretin amyloid cardiomyopathy: JACC state-of-the-art review. Journal of the American College of Cardiology, 73(22), 2872–2891. https://doi.org/10.1016/j.jacc.2019.04.003
7Lane, T., Fontana, M., & et al. (2019). Natural history, quality of life, and outcome in cardiac transthyretin amyloidosis. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.118.038169
8Sattar, Y., & Chhabra, L. (2023). Electrocardiogram. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK549803/
9InformedHealth.org. (2024). In brief: What is an echocardiogram? Institute for Quality and Efficiency in Health Care (IQWiG). https://www.ncbi.nlm.nih.gov/books/NBK395556/
10Dorbala, S., Ando, Y., & et al. (2021). ASNC/AHA/ASE/EANM/HFSA/ISA/SCMR/SNMMI expert consensus recommendations for multimodality imaging in cardiac amyloidosis: Part 1 of 2—Evidence base and standardized methods of imaging. Circulation: Cardiovascular Imaging, 14(7). https://doi.org/10.1161/hci.0000000000000029
11Amyloidosis Research Consortium. (2023). Expanded diagnoses outside of specialized amyloidosis centers: Results from the Amyloidosis Research Consortium’s 2022 community survey. Presented at ISPOR, Boston, MA, USA. Available at PowerPoint Presentation (arci.org)
12Nativi-Nicolau, J. N., Karam, C., Khella, S., & Maurer, M. S. (2022). Screening for ATTR amyloidosis in the clinic: Overlapping disorders, misdiagnosis, and multiorgan awareness. Heart Failure Reviews, 27(3), 785–793. https://doi.org/10.1007/s10741-021-10080-2
13Bruno, M., Castaño, A., Burton, A., & Grodin, J. L. (2021). Transthyretin amyloid cardiomyopathy in women: Frequency, characteristics, and diagnostic challenges. Heart Failure Reviews, 26(1), 35–45. https://doi.org/10.1007/s10741-020-10010-8
14Aimo A., Tomasoni D., et al. Left ventricular wall thickness and severity of cardiac disease in women and men with transthyretin amyloidosis. Eur J Heart Fail, 25: 510-514. https://doi.org/10.1002/ejhf.2824 (2023)
15Aimo A., Panichella G., Garofalo M., et al. Sex differences in transthyretin cardiac amyloidosis. Heart Fail Rev 29, 321–330 (2024). https://doi.org/10.1007/s10741-023-10339-w
16Kaiser Family Foundation. (2023). Women’s experiences with provider communication & interactions in health care settings: Findings from the 2022 KFF women’s health survey. https://www.kff.org/womens-health-policy/issue-brief/womens-experiences-with-provider-communication-interactions-health-care-settings-findings-from-2022-kff-womens-health-survey/
17Patel, R. K., Fontana, M. & et al. (2022). Sex differences among patients with transthyretin amyloid cardiomyopathy – from diagnosis to prognosis. European journal of heart failure, 24(12), 2355–2363. https://doi.org/10.1002/ejhf.2646
18Lauppe, R. E., Hansen, J. L., Gerdesköld, C., & et al. (2021). Nationwide prevalence and characteristics of transthyretin amyloid cardiomyopathy in Sweden. Open Heart, 8, Article e001755. https://doi.org/10.1136/openhrt-2021-001755
PP-VDM-USA-1981 October 2024
